Introduction:
Literature review can be explained as the segment of a dissertation or a thesis that comprises of an exhaustive review of literatures that has already been done and closely relate to the research topic (Aveyard 2014). This section would include an exhaustive review of scholarly literatures that are aligned to the research objectives. Typically the scholarly literatures included in the review were published in between 2010 to 2018. The rationale for the inclusion of papers published over 9 years include a detailed overview about what has already been done in the research area of interest.
1.1: Review of literatures:
Research studies mention that fibrosis includes the formation of a large amount of scar tissue in the liver (Sumida et al. 2014). The condition arises when the liver repairs and regenerates its damages cells. It should be noted in this context that a number of conditions can damage the liver. Further, as stated by Zeybel and Idilman (2018), fibrosis does not typically trigger any symptoms but excessive scarring can result in cirrhosis which can worsen the intensity of the symptoms. Fibrosis can be detected on the basis of blood and imaging tests, however on certain occasions liver biopsy can help in detecting fibrosis (Fallatah 2014). The condition can be treated with the implementation of a number of medical treatment.
Fibrosis manifests when the liver gets continuously damaged. It should be noted in this context that a single event of injury does not lead to fibrosis. Liver fibrosis manifests itself when the injury is repetitive and results in the formation of a scar tissue (Castera and Pinzani 2010). In cases where the injury is repetitive and continuous the hepatic cells or the liver cells attempt to recover the damaged tissue but the attempt to repair and recover the damaged tissue leads to the formation of a scarred tissue (Hernandez-Gea and Friedman 2011). Fibrosis is generally formed when a blockage is formed within the bile ducts (Friedrich-Rust et al. 2008). The scar tissues that are formed replace the hepatic cells and do not perform any important metabolic function. Also, scarring leads to distortion of the internal structure of the liver. It should be crucially noted in this context that widespread and controlled scarring and distortion lead to cirrhosis. In other words, it can be said that fibrosis and cirrhosis are not specific disorder but are other primary causes that lead to liver damage (Wallace et al. 2008). The scar tissues that are formed interfere with the blood flow to the liver and limits the blood supply to the hepatic tissues (Friedrich-Rust et al. 2008). On account of lack of appropriate blood supply, more scar tissues are formed and the condition elevates the blood pressure in the hepatic portal vein that is responsible for carrying the blood from the intestine to the liver. This condition is also known as portal hypertension. Research studies suggest that the condition of Fibrosis can be reversed only if the condition is diagnosed early and appropriate treatment regimen is followed so as to ensure recovery (Zeybel and Idilman 2018; Castera and Pinzani 2010)).
The condition is triggered by a broad spectrum of drugs that continuously damage the liver and cause liver fibrosis. These drugs mostly include Alcohol Amiodarone, Chlorpromazine, Corticosteriods, Isoniazid, Methotrexate, Methyldopa, Oxyphenisatin and Tolbutamide (Wallace et al. 2008). The mentioned drugs are mainly processed in the liver and therefore can interfere with the normal functioning of the liver. In addition to this, a number of other factors such as congenital disorders including congenital hepatic fibrosis and Non-alcoholic fatty liver can also elevate the risk of suffering from Liver Fibrosis. Research studies reveal that congenital hepatic fibrosis typically damage the kidneys, gallbladder and the liver (Schuppan and Kim 2013; Tacke and Zimmermann 2014). The disorder is present at birth and also leads to the manifestation of a number of symptoms. In case of the second most common disorder, or the Non-alcoholic fatty liver, the fat accumulates within the liver which leads to the development of fibrosis (Lee et al. 2015). The disorder is more common in people who suffer from metabolic syndrome. A number of other physiological problems can enhance the probability of suffering from Liver fibrosis. Scholarly literature suggests that a number of genetic metabolic disorders can increase the risk of suffering from Liver Fibrosis (Tacke and Zimmermann 2014). Patients that suffer from Alpha-1 antitrypsin deficiency OR Iron Overload hemochromatosis or Wilson disease are twice more likely to suffer from Liver Fibrosis. These genetic disorders typically manipulate the manner in which nutrients are broken down, metabolised or assimilated within the body (Puche et al. 2011). In cases where the nutrients are not metabolized in a synchronised manner, there could be a possibility that the substances would accumulated within soft tissue organs such as the liver which could lead to scarring. Further, the evidence base also suggests that viral infections like chronic hepatitis B or C can adversely affect the liver which could give rise to scarring of hepatic tissues (Shah et al. 2009). Also, the risk of suffering from liver fibrosis increases in patients who suffers from autoimmune disorders. These autoimmune disorders include problems such as Auto-immune hepatitis Primary biliary, Cholangitis and Primary Sclerosing Cholangitis (Iwaisako et al. 2012). On being affected with these autoimmune disorders, the body has a tendency to act against its own immune system. This increases the probability of scarring the hepatic tissues. In the mentioned autoimmune disorders, the bile duct is inflamed with scarring of tissues and blockage. Further, liver fibrosis also manifests in cases where the hepatic blood flow is interrupted. In case of Budd-Chiari syndrome, a blood clot interrupts the blood flow out of the liver (Parkes et al. 2010). Further, in case of Heart failure or Portal Vein thrombosis, the main vein that supplies blood to the liver is blocked by a blood clot. In case of Veno-occlusive disease of the liver, the small veins of the liver are blocked by the presence of blood clot and this leads top scarring of the hepatic tissues (Bejarano et al. 2009). It should be noted in this context that in conditions where the blood is unable to leave the liver, the liver gets inflamed and the size of the liver enlarges. Also, due to lack of sufficient blood supply, the hepatic cells die and are continuously replaced with the scar tissues. Also, scarring can be caused due to Sinusoidal obstruction syndrome. The Sinusoidal obstruction syndrome is caused by the accumulation of pyrrolizidine alkaloids (Cales et al. 2009). These alkaloids are present in a number of herbal products which include supplements and herbal tea extracts which are considered beneficial for the physical health of individuals (Mallet et al. 2009).
The evidence base further enlist the most common causes to be alcohol abuse, viral hepatitis C and Nonalcoholic fatty liver which lead to Liver fibrosis within the U.S population base (Poynard et al. 2012). In this regard, it is important to note that Non-alcoholic fatty liver in generally occur in individuals who are obese, are either pre-diabetic or are diagnosed with Diabetes (Mallet et al. 2009). Further, increase in level of cholesterol or lipid within the blood serve as high risk factors that lead to Liver Fibrosis.
According to Cales et al. (2009), it has been mentioned that scarring forms the first stage of Liver fibrosis. If the scarring of the hepatic tissue is uncontrolled then liver Fibrosis can assume a more serious forms which is also known as Liver Cirrhosis. It is important to note in this context that research done on a number of animal trials have successfully proven that the damaged liver has the capability to regenerate itself (Bejarano et al. 2009). However, unfortunately, the same has not been researched in human models. As a matter of fact, the research conducted on humans show that once there is scarring within the liver tissue, the hepatic tissue do not reveal or regenerate at an accelerated pace (Parkes et al. 2010). However, a number of lifestyle modifications can help in preventing the fibrosis from getting worse and ensure proper symptom management. It is on the basis of staging that the physician estimates the percentage of liver damage (Bejarano et al. 2009). It is important to acknowledge in this context that staging is subjective and every scale has its own set of limitations. The most prevalent scoring system is the METAVIR scoring scale. The system helps in predicting the degree at which the scarring of the tissues or fibrosis is spreading. Physicians generally assign the score after performing the biopsy on a tissue sample. Also, the activity grades range invariably in between the scores A0 to A3. A0 suggests no activity, A1 suggests mild activity, A2 suggests moderate activity and As suggests severe activity (Iwaisako et al. 2012). The fibrosis stages are marked in between the range of F0 to F4. F0 suggests no fibrosis, while F1 suggests portal fibrosis without septa. F2 suggests portal fibrosis with few septa, F3 suggests a number of septa without the indication of Cirrhosis and F4 suggests Cirrhosis (Mallet et al. 2009). Therefore, on the basis of grading discussed, a patient that suffers from the most severe form of the disease would be scored A3, F4 METAVIR score.
The scoring system propounded by Batts and Ludwig is one of the other scoring system that marks Liver Fibrosis in a range of grade 1 to grade 4. Grade 4 marks the most severe form of Liver Cirrhosis. Some of the most common symptoms of Liver Fibrosis include, loss of appetite, distortion of thoughts, fluid accumulation within stomach or legs, nausea, weight loss, weakness and Nausea. A research study conducted by Shah et al. (2009), reported that almost 6% to 7% of the World population suffers from Liver Fibrosis but is not aware of the same.
The most common treatment options comprise of implantation of pharmacological interventions such as using ACE inhibitors like Lisinopril, Ramipril and Benazepril. In addition to this treating with a Tocopherol or interferon-alpha and PPAR-alpha agonist can also help in treating Liver Fibrosis (Puche et al. 2011).
The introduction of the clinical discipline of Hepatology coincides with Menghini’s needle in the early 1950s. Liver biopsy was the only diagnostic method available in this regard, and it really was a gold standard with regard to the identification of liver fibrosis. From the start it was characterized by an extensive cooperative attempt between the doctor and pathologist to introduce the so called one second needle biopsy of the liver (Bejarano et al. 2009). Liver biopsy is the more accurate method to identify and detect fibrosis (to determine the degree of severity) and to recognize the fibrosis-related disease. When the diagnosis is uncertain, biopsy is often performed. Due to invasive nature of the liver biopsy which can trigger complications, physicians can do blood tests first to determine the degree of fibrosis and then conduct liver biopsy if only blood tests show a mild or serious amount of fibrosis. Recent evidence suggests medical professionals use certain specific imaging tests more and more as non-invasive biopsy options (Tacke and Zimmermann 2014). The use of hepatic biopsy was a step forward with the implementation of scouring technologies. This introduction meant that the evaluation of liver biopsy specimens which was beyond characterization and, in many cases, the view of the pathologist had been made more accurate. In general, it was intended to promote the implementation of scoring schemes in the context of a worldwide contract to compare sample outcomes (Schuppan and Kim 2013). In fact, liver biopsy is vulnerable to intra-observer and inter-observer variability and sampling mistakes. Even a 25 mm lengthy liver biopsy, for example, has a 25 per cent fibrosis discord. In addition, if the size of the specimen is sufficient, the experience of the pathologist becomes even more important with respect to specialization, length and place of exercise (Wallace et al. 2008).
The liver biopsy doesn’t effectively mirror the fibrotic changes taking place throughout the liver, as an efficiently formed biopsy contains 5 to 11 full portal tracts and represents only 1/ 50000 liver volume (Hernandez-Gea and Friedman 2011). The hepatic fibrotic process is not linear and there have been different stages of fibrotic biopsies from different regions. In 10 to 30 per cent of patients it was shown in several reports that cirrhosis could be missed. Early and advanced end- stage cirrhosis cannot distinguish a liver biopsy and cannot thus be used as an optimal prognostic predictor (Castera and Pinzani 2010). With regard to the liver biopsy complications, pain incidences are reported to be 20 per cent, but they grow to 84 per cent if they include a slightly uncomfortable sensation. The occurrence was revealed to be 0.3 per cent -0.57 per cent and 0.01 per cent respectively of severe complications and mortality. Operators who are trained by an experienced teacher should conduct a biopsy to minimize complications and it is advisable to operate with an American guide and use an aspirative type of biopsy needle (Castera and Pinzani 2010). In addition to the fat deposits of the typical NASH (non -alcoholic steatohepatitis) in hepatocytes, the pathological features of the NSAH include inflame cells (neutrophils and lymphocytes), lobula infiltrations, hepatocytic degradation by balloning, Mallory – Denk bodies, fibrosis pericellular, sinusoidal fibrosis. However, few patients with NASH demonstrate all these typical results, and NASH diagnosis on the basis of them does not have embedded requirements. Studies categorized NAFLD as 4 kinds: type 1, (only fat deposition), type 2, (fat exposure and parenchyma inflammatory cell infiltration), type 3, (fat accumulation and hepatocytes ballon degeneration), and type 4, (type 3 requirements as well as Mallory -Denk bodies and/ or fibrosis). Researchers noted that liver disease-related mortality in the type 1 plus type 2, but increased considerably to 11 per cent in type 3 plus type 4, were only 1.7 per cent in the follow -up era of roughly eight years (Toyoda et al. 2011). From a predictive point of view, they suggested defining the kinds 3 and 4 as NASH. Liver biopsies can be carried out in ambulatory hospitals to decrease cost abroad, but patients with biopsy are hospitalized in Japan for a few days. Liver biopsies, approximately valued at 10 million for all patients in Japan, would not be very cost effective for all NAFLD patients. However, there have been no cost-benefit analyses to date. With respect to follow – up after liver biopsy, Toyoda et al. (2011) noted that NAFLD patients have a very low follow-up frequency, compared with that of viral hepatitis patients.
Several comprehensive Western country reviews have earlier discussed non – invasive NASH or advanced fibrosis diagnostic techniques. Most of these articles however outlined a straightforward list of non – invasive trials. Thus, in this research investigation, biomarkers or scoring schemes with critical evaluations will be discussed as well as diagnostic algorithms that can be applied even in clinical practice in NAFLD patients (Puche et al. 2011). NIMs (Non- invasive Markers) help evaluate the stage of fibrosis in patients with no clear evidence of liver biopsy, for example patients with CHB (chronic hepatitis B), persistent normal fibrous alanine aminotransferase serum (ALT), patients with CHC (chronic hepatitis C) or CHB who require further assessment of fibroid stage during or following treatment, and patients with autoimmune hepatitis (AIH) who have experienced r-induced fibroid phases. In order to use serum markers directly associated to the fibrogenic system, known as “direct markers” (such as hyaluronic acid, TIMP1 or Tissue Inhibitor of Metalloproteinase 1), patients with other chronic illnesses that are characterized by fibro- genesis or changing extracellular in other bodies and structures should cautiously be ruled out. Even though patient age has never fully researched the effect of direct serum markers, the restricted proof available still shows that in a paediatric cohort the same direct markers are more sensitive and particular than in the adult NAFLD (Non -alcoholic fatty liver disease) cohort (Shah et al. 2009). The mixed serum biomarker diagnostic significance for hepatic fibrosis was identified in one research. 182 chronic hepatitis C infected patients from several Turkish facilities were included in the research. There were two categories of patients: mild stage fibrosis (Metavir, F0 – F1) or advanced stage fibrosis (Metavir, F2 – F4) (Puche et al. 2011). Two categories included. Of the trials examined, the sensitivities in APRI, FIB-4 and Fibrotest for serious fibrosis were 69 per cent, 69 per cent and 75 per cent, respectively, with specificity of 60 per cent and 71 per cent, respectively.
Liver fibrosis NIBMs (Non – invasive Biomarkers) are divided into two main categories: Class 1 or direct biomarkers or fibrosis markers, or indirect biomarkers. The immediate markers correspond directly with the fibrosis method, or are components of the Hepatic stellate cells matrix generated during ECM turnover (Schuppan and Kim 2013). The indirect markers, on the other hand, represent changes in the function of the liver and are molecules emitted into the blood owing to swelling of the liver. Procollagen is a precursor of collagen. The carboxy – terminal (Type 1 (PC1CP)) is cleaved with two distinct enzymes, which produce collagen and the amino -terminal (Type III (PCIIINP). Collagen mature is integrated in the ECM. Type IV collagen is a ECM element examined as a liver fibrosis replacement marker. It has three distinct areas (a domain of the amino -terminal, a core helix and a carboxy – terminal (Tacke and Zimmermann 2014). Collagen Type IV has been widely researched in various etiological liver diseases. Hyaluronic acid (HA) is a element of the EMC generated by hepatic stellate cells and a glycosaminoglycan. Laminine has been generated by hepatic star cells as a non – collagen glycoprotein element of ECMs. It is placed in the membrane of the liver cellar. Serum laminin concentrations, as described by distinct writers, are raised beyond the ordinary upper limit (0.59 to 1.4 U / mL) or (9.74 to 2.46) (Bejarano et al. 2009).
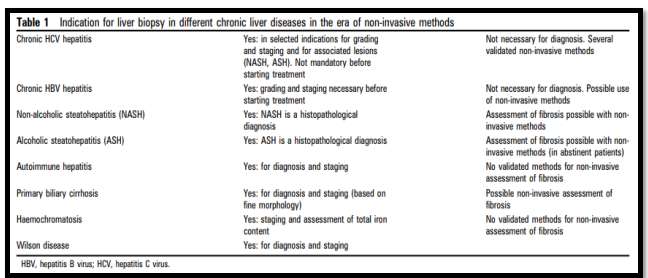
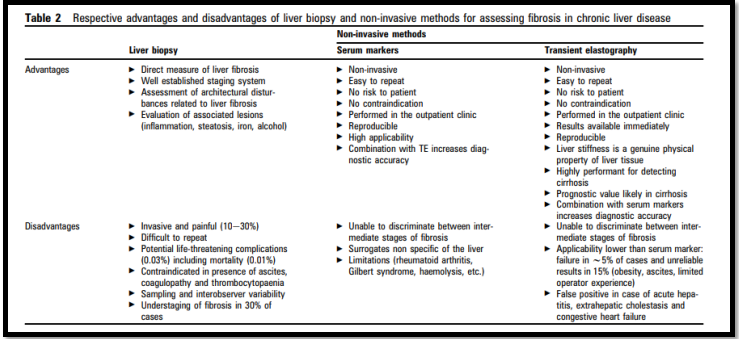
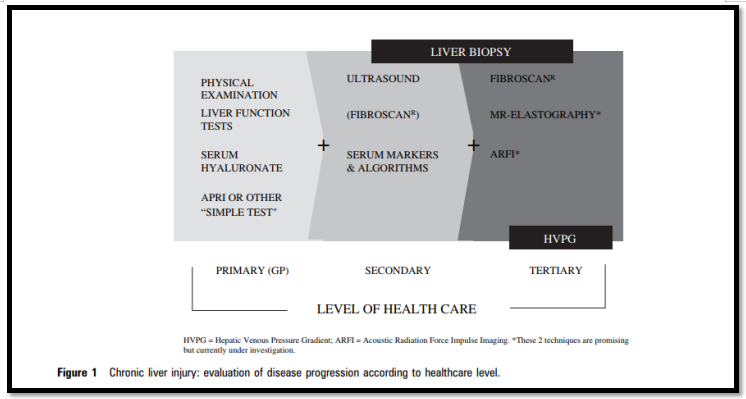
(Source: Castera and Pinzani 2010)
(Source: Castera and Pinzani 2010)
(Source: Castera and Pinzani 2010)
Serum alanine aminotransferase or ALT is among the earliest markers used to evaluate liver disease. Studies have shown that serum ALT is good for measurement because of its elevated sensitivity and special characteristics (2.25 times larger than ordinary headache histology predicts). Serum ALT concentrations are however influenced by a number of variables such as the sex, the body mass index and the use of hepatotoxic medicines. One of the oldest and most readily accessible markers of liver fibrosis is the aspartate aminotransferase (AST)/ALT (AAR) ratio (Cales et al. 2009). It has been reinforced for various types of hepatic disease and a ratio higher than one is cirrhosis predictive. A 1.16 AAR was discovered to forecast high -precision one -year mortality. The BARD rating involves the BMI AAR and diabetes testing, which Harrison et al. suggested in 2008. It showed an increased efficiency of NPVs of 96 per cent and 81.3 per cent relative to the NFAS (Patel et al. 2004).
With regard to the Proteomics and glycomics, mass spectrometry is used for the evaluation of proteins and glycoproteins. Primary proteomics and liver fibrosis studies showed promising outcomes using serum samples. However, latest information showed that the evaluation of liver fibrosis with these techniques is of restricted importance.Several researchers have tried to combine NIMs for the evaluation of hepatic fibrosis, suggesting enhanced sensitivity. Several trials comparing various algorithms combining direct NIBMs were performed. For various NIBM combinations, the bulk of the research showed similar outcomes. Moreover, compared to individual markers, the combined algorithms showed considerably better performance. Patel et al. (2004) suggested a combined algorithm of distinct non – invasive direct markers. For fibrosis evaluation in CHC patients, this study mixed hyaluronic acid, TIMP-1 andα2-macroglobulin to demonstrate a 75 per cent precision in the identification of fibrosis F2 – F4. More lately, the superiority of APRI to AAR has been verified in the identification of both advanced fibrosis and cirrhosis in a research of both CHC and CHB patients with hepatocellular carcinoma postresection. In one research, distinct NIBM combinations for evaluating fibrosis in CHC by using six non – invasive trials showed the highest performance with 0.86 and 0.84 respectively, followed by fibro testing. The Forns Index and Hepascore, on the other hand, have shown lower results, respectively AUCs of 0.78 and 0.79. Compared with Fibrospect II, the Fibro test in individuals with HCV genotype 1 was discovered to be more exact and cost efficient.
Because of the following reasons, NIBMs are beneficial compared with liver biopsies. They are non-invasive and measurable in ambulatory services. Compared to liver biopsies, they cost less. For confirmation, they can readily be repeated. They can be used for follow – up and monitoring in the future if they are well validated. They are not connected with liver biopsy co-morbidity and risks of death (Iwaisako et al. 2012).
In intermediate phase of liver fibrosis, some markers such as APRI, HePascore and Fibrospect II require more validation. Despite the fact that NIBM’s efficacy has been demonstrated in numerous studies, certain studies showed that it cannot be diagnostic in the identification of liver fibrosis (Shah et al. 2009). There remains little value to evaluate the growth of complications such as oesophageal varicose veins and the possibility of variceal bleeding. Both direct and indirect hepatic fibrosis markers are not hepatic and can be affected in other organs by pathological circumstances. Because of variable values and the distinct top normal ranges of the various laboratories, some biomarkers have no standardization. The hepatic biopsy is also a restriction in all the trials evaluating the precision of NIBMs, as the protocol also preserves the danger of sampling mistake, even when best biopsy has been conducted (Lee et al. 2015). A predictive distortion of the population studied can bias the outcomes, which will influence the accurateness of the markers, for instance if a greater proportion of individuals with advanced or minimum fibrosis are included (Schuppan and Kim 2013).
NIBMs can be used to evaluate the development of illness and to predict patients with liver cancer complications and survival. Treatment answers can be monitored by NIBMs. Due to its complications, the screening for high risk groups like CHB patients with normal liver enzymes and overweight or diabetic patients with anticipated NAFLD cannot be performed with the hepatic biopsy (Zeybel and Idilman 2018). Thus, these patients can be screened using NIBMs. Given the above constraints and patients falling into grey fields with the use of non-invasive markers, liver biopsy remains needed to diagnose patients such as patients suffering from viral hepatitis B and C, and secondary diagnoses such as NAFLD, AIH, or ALD. Likewise, the option of NAFLD or autoantibody – negative AIH may be endorsed or excluded by liver biopsy in patients who do not test for viral markers and auto – antibodies (Sumida et al. 2014). Additionally, the use of non – invasive markers was not well assessed for toxic liver damage, such as methotrexate caused hepatic injury.
1.2: Discussion:
Therefore, on the basis of the exhaustive review of literatures a number of key findings could be derived which would be discussed under common repetitive themes.
Diagnosis and Scoring of Liver Fibrosis:
Research papers included in the review mentioned that Physicians commonly used the METAVIR scoring system for determining the level of scoring or estimating the speed at which the scarring is progressing within the hepatic tissue. The activity range is generally marked in between the grade A0 to A3. Ao refers to no activity, A1 represents mild activity, A2 represents moderate activity and A3 represents severe activity (Castera and Pinzani 2010). Also, the fibrosis stages are marked in between F0 to F4. Fo suggests no fibrosis, F1 represents portal fibrosis without the presence of septa, F2 represents portal fibrosis with some septa, F3 represents numerous septa without Cirrhosis and F4 represents Cirrhosis (Fallatah 2014). Another scoring system is also used by physicians which is known as the Batts and Ludwig scale and it critically rates the fibrosis from grade 1 to 4.
Factors that increase the risk of suffering from Liver Fibrosis:
On critically evaluating the evidence base, it can be said that a number of risk factors influence the probability of suffering from Liver Fibrosis. These factors include lifestyle and nutritional factors such as excessive alcohol consumption, being over-weight or consuming a diet high in lipid content (Zeybel and Idilman 2018). In addition to this, a number of other factors increase the risk of being affected from the disorder and this includes, chronic illness history such as suffering from Diabetes, Fatty liver disease or suffering from Diabetes (Puche et al. 2011). In addition to this, the evidence base also suggests that the disorder is triggered by a number of factors that include a previous history of autoimmune disorder, infection or genetic disorders that interfere with the hepatic blood circulation. These factors increase the probability of scarring of hepatic tissues which when left untreated could also lead to cirrhosis (Friedrich-Rust et al. 2008).
Molecular diagnostic methods for diagnosis of Liver fibrosis:
The evidence base suggests that Liver Fibrosis Biomarkers are used for testing and diagnosis of Liver fibrosis. In this regard, it should be noted that the Non-invasive biomarkers are majorly divided into sub categories that include class 1 or direct biomarkers and indirect biomarkers (Iwaisako et al. 2012). The immediate markers correspond directly with the fibrosis method, or are components of the Hepatic stellate cells matrix generated during ECM turnover. The indirect markers, on the other hand, represent changes in the function of the liver and are molecules emitted into the blood owing to swelling of the liver (Wallace et al. 2008). Procollagen is a precursor of collagen. Further, With regard to the Proteomics and glycomics, mass spectrometry is used for the evaluation of proteins and glycoproteins. Primary proteomics and liver fibrosis studies showed promising outcomes using serum samples. NIBMs have been considered beneficial compared with liver biopsies as they are non-invasive and conveniently measurable in ambulatory services (Castera and Pinzani 2010).
1.3: Research Gap:
Therefore, on the basis of the review of literatures, a gamut of information could be extracted in relation to Liver Fibrosis. The papers included in the review critically presented detailed information about the lifestyle and dietary factors that elevate the risk of suffering from Liver Fibrosis. In addition to this, the included scholarly literature also talked about the common symptoms that manifest on being affected with Liver Fibrosis. The review of literature also helped in developing an understanding about the grading of scarring of tissues which helps Physicians determine the extent to which the disease has progressed. In addition to this, some of the papers also shed light on the molecular diagnostic methods that are used for diagnosis of the disease. A research gap was typically found in terms of recent research papers that have focused on the research topic. This accounted for the reason why a number of secondary research articles had to be considered for the review. Another, research gap can be mentioned in terms of recent pharmacological interventions and breakthrough treatment that can help in treating the disorder. Therefore, the research conducted by the research would primarily focus on the identified literature gap and aim to address the gap with the collected research evidence.
1:4: Summary:
Therefore, to summarise it can be mentioned that the literature review helped in identification of a number of scholarly literatures that define Liver Fibrosis as a disorder and mention its common symptoms to be loss of appetite, sudden weight loss, nausea and weakness. In addition to this, the review of literatures also present an overview about the methods of diagnosis to confirm and grade the disorder. Further, the research review also mentions about a number of molecular diagnostic methods can help in identification of the correct stage of liver fibrosis. However, the review of literatures lacks inclusion of primary research studies that talk about breakthrough treatment methods and pharmacological treatments which can help in curing the disorder.
Methodology:
2.0: Introduction:
According to Austin (2011), methodology forms an integral chapter of a thesis or a dissertation that outlines the research method that would be followed while conducting the research. This chapter enables the researcher to select an appropriate research methodology from the evidence base which would help in addressing the articulated research question and the research objectives.
2.1: Data Collection Method:
2.2: Search Strategy:
In order to address the literature review section, an exhaustive search on the electronic databases was conducted. This was done in a methodological manner and with the use of specific key words that were aligned to the articulated research objectives. It should be noted in this context that the exhaustive search of literatures was conducted on the electronic database of CINAHL, Google Scholar and MedLine. The justification for the choice of electronic databases can be explained as medical databases that house a gamut of literature relevant to human physiology and disorders.
PRISMA:
Screenshots of search results:
2.3: Inclusion criteria:
As stated by Aveyard (2014), a set of inclusion criteria helps in retrieving relevant research studies that are aligned with the selected research topic. In this case, the inclusion criteria that was considered included the following:
- Research papers published in English were considered for the literature review
- Research papers published in between 2008 to 2019 were considered for the review
- Research papers that covered a research breakthrough technique was also considered for the review even if the publication was before the year 2008
- Papers that were published in reputed journals were considered
- Papers that were accessible for full text was considered for the review
2.4: Exclusion Criteria:
As mentioned by Bergh and Ketchen (2011), a set of exclusion criteria critically includes the set of characteristics that are used to exclude or filter research papers that are not relevant to the research review. In this case, the following exclusion criteria was followed:
- Research papers that were published in foreign languages other than English
- Research papers that were not accessible for full text
- Research papers that included animal trials
- Research papers that were published before 2008
2.5: Key words:
As per Bettany-Saltikov (2012), keywords are short condensed phrases that are strongly aligned with the research question. Identification of appropriate key words are important so that relevant research papers can be retrieved from the electronic database. In this case, the following list of key words were used:
Liver Fibrosis, Diagnosis, Symptoms, Molecular technique, Biomarkers, molecular testing, prognosis, pitfalls in markers, Genetic markers, sequential algorithms, risk factors, stages of liver fibrosis, liver cirrhosis.
The listed key terms were searched on the electronic databases using Boolean operators OR/AND as the use of Boolean operators on electronic databases help in retrieving the most relevant research studies (Boland et al. 2014). The key words were thus searched in combination with one or both Boolean operators, for example, Liver Fibrosis AND/OR Genetic Markers. This helped in retrieving the most relevant and appropriate research journal that was close to the research topic.
2.6: Snowball Technique:
As stated by Catherine Houghton et al. (2013), the electronic databases contain a gamut of scholarly evidences and are updated regularly which makes it possible that certain important research articles are overlooked for inclusion in the review. In order to solve this problem, Coughlan et al. (2013) stated that scanning of the reference lists of the retrieved research papers for inclusion in the review can help in making the review more credible and authentic. This method of scanning the reference section of the selected articles for inclusion in the review is known as the snowball technique. In this case, a total of 10 articles were retrieved on the basis of snowball technique.
2.7: Assessment of Quality:
The assessment of quality was done by reading the title of selected research papers. Further the abstract of the research papers were thoroughly read and re-read. Research papers that did not satisfy the inclusion criteria were excluded. This led to the inclusion of 30 articles. The next criterion that was considered included evaluation of the sample size. The articles that comprised of a substantial sample size such that the results could be generalised was included and this led to the inclusion of a total of 15 articles. The rationale for the exclusion of articles with poor sample size was to avoid research bias.
2.8: Research Philosophy:
According to Creswell and Clark (2017), a total of three research philosophies exist which comprises of positivism, interpretivism and realism. In this case, the interpretivism philosophy has been followed as it is appropriate for qualitative research type. The philosophy helps in analysing stipulated and condensed data, as only 15 articles were selected, the interpretivism philosophy would be appropriate for this research study.
2.9: Research Approach:
Research studies suggest that a total of two research approach methods are used by researchers while addressing a research study (Crowther and Lancaster 2012). These methods include inductive and deductive approach. While the inductive approach emphasised on the generation of new theory, the deductive theory tests the pre-existing notion about a theory. In this case, the inductive research approach would be chosen.
2.10: Research Design:
A total of three types of research designs are used for conducting research studies and this includes exploratory, explanatory and descriptive type of research design (Ellis and Levy 2012; Crowther and Lancaster 2012). In this case, the researcher would adapt the descriptive type of research study design as the research intends to deduce themes to discuss what has been researched and has been added to the evidence base.
2.11: Conclusion:
Therefor to conclude, it should be mentioned that the researcher would adapt a qualitative research design with an inductive approach and make use of positivism research philosophy. Further the researcher would adapt a descriptive style of research design and make use fop 15 articles to critically address the literature review.
References:
Austin, P.C., 2011. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate behavioral research, 46(3), pp.399-424.
Aveyard, H., 2014. Doing a literature review in health and social care: A practical guide. McGraw-Hill Education (UK).
Bejarano, G., Vergara, M., Gil, M., Dalmau, B., Puig, J., Bella, M.R., Suárez, D. and Calvet, X., 2009. Prospective evaluation of liver fibrosis in chronic viral hepatitis C infection using the Sabadell NIHCED (non-invasive hepatitis C related cirrhosis early detection) index. Revista Espanola de Enfermedades Digestivas, 101(5), p.325.
Bergh, D., and Ketchen, D. J., 2011. Research methodology in Strategy and Management, 1st ed. Bingley: Emerald Group Publishing Ltd
Bettany-Saltikov, J., 2012. How to do a systematic literature review in nursing: a step-by-step guide. McGraw-Hill Education (UK).
Boland, A., Cherry, M G and Dickson, R. 2014. Doing a systematic review : a student’s guide. Sage Publications. London.
Calès, P., Lainé, F., Boursier, J., Deugnier, Y., Moal, V., Oberti, F., Hunault, G., Rousselet, M.C., Hubert, I., Laafi, J. and Ducluzeaux, P.H., 2009. Comparison of blood tests for liver fibrosis specific or not to NAFLD. Journal of hepatology, 50(1), pp.165-173.
Castera, L. and Pinzani, M., 2010. Biopsy and non-invasive methods for the diagnosis of liver fibrosis: does it take two to tango?.
Catherine Houghton, R.G.N., Dympna Casey, R.G.N. and David Shaw PhD, C., 2013. Rigour in qualitative case-study research. Nurse Researcher (through 2013), 20(4), p.12.
Coughlan, M., Cronin, P. and Ryan, F., 2013. Doing a Literature Review in Nursing, Health and Social Care: SAGE Publications. Sage.
Creswell, J.W. and Clark, V.L.P., 2017. Designing and conducting mixed methods research. Sage publications.
Crowther, D., and Lancaster, G., 2012. Research Methods, 2nd ed. London: Routledge.
Ellis, T., and Levy, Y., 2012. ‘Towards a guide for novice researchers on research methodology: Review and proposed methods’, Issues in Informing Science and Information Technology, 6, 323-337.
Fallatah, H.I., 2014. Noninvasive biomarkers of liver fibrosis: an overview. Advances in Hepatology, 2014.
Friedrich–Rust, M., Ong, M.F., Martens, S., Sarrazin, C., Bojunga, J., Zeuzem, S. and Herrmann, E., 2008. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology, 134(4), pp.960-974.
Harrison, S.A., Oliver, D., Arnold, H.L., Gogia, S. and Neuschwander-Tetri, B.A., 2008. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut, 57(10), pp.1441-1447.
Hernandez-Gea, V. and Friedman, S.L., 2011. Pathogenesis of liver fibrosis. Annual review of pathology: mechanisms of disease, 6, pp.425-456.
Iwaisako, K., Brenner, D.A. and Kisseleva, T., 2012. What’s new in liver fibrosis? The origin of myofibroblasts in liver fibrosis. Journal of gastroenterology and hepatology, 27, pp.65-68.
Lee, Y.A., Wallace, M.C. and Friedman, S.L., 2015. Pathobiology of liver fibrosis: a translational success story. Gut, 64(5), pp.830-841.
Mallet, V., Dhalluin‐Venier, V., Roussin, C., Bourliere, M., Pettinelli, M.E., Giry, C., Vallet‐Pichard, A., Fontaine, H. and Pol, S., 2009. The accuracy of the FIB‐4 index for the diagnosis of mild fibrosis in chronic hepatitis B. Alimentary pharmacology & therapeutics, 29(4), pp.409-415.
Parkes, J., Roderick, P., Harris, S., Day, C., Mutimer, D., Collier, J., Lombard, M., Alexander, G., Ramage, J., Dusheiko, G. and Wheatley, M., 2010. Enhanced liver fibrosis test can predict clinical outcomes in patients with chronic liver disease. Gut, 59(9), pp.1245-1251.
Patel, K., Gordon, S.C., Jacobson, I., Hézode, C., Oh, E., Smith, K.M., Pawlotsky, J.M. and McHutchison, J.G., 2004. Evaluation of a panel of non-invasive serum markers to differentiate mild from moderate-to-advanced liver fibrosis in chronic hepatitis C patients. Journal of hepatology, 41(6), pp.935-942.
Poynard, T., Lenaour, G., Vaillant, J.C., Capron, F., Munteanu, M., Eyraud, D., Ngo, Y., M’kada, H., Ratziu, V., Hannoun, L. and Charlotte, F., 2012. Liver biopsy analysis has a low level of performance for diagnosis of intermediate stages of fibrosis. Clinical Gastroenterology and Hepatology, 10(6), pp.657-663.
Puche, J.E., Saiman, Y. and Friedman, S.L., 2011. Hepatic stellate cells and liver fibrosis. Comprehensive Physiology, 3(4), pp.1473-1492.
Schuppan, D. and Kim, Y.O., 2013. Evolving therapies for liver fibrosis. The Journal of clinical investigation, 123(5), pp.1887-1901.
Shah, A.G., Lydecker, A., Murray, K., Tetri, B.N., Contos, M.J., Sanyal, A.J. and Nash Clinical Research Network, 2009. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clinical Gastroenterology and Hepatology, 7(10), pp.1104-1112.
Sumida, Y., Nakajima, A. and Itoh, Y., 2014. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World journal of gastroenterology: WJG, 20(2), p.475.
Tacke, F. and Zimmermann, H.W., 2014. Macrophage heterogeneity in liver injury and fibrosis. Journal of hepatology, 60(5), pp.1090-1096.
Toyoda, H., Kumada, T., Kiriyama, S., Tanikawa, M., Hisanaga, Y., Kanamori, A. and Tada, T., 2011. Markedly lower follow-up rate after liver biopsy in patients with non-alcoholic fatty liver diseases than those with viral hepatitis in Japan. BMC research notes, 4(1), p.341.
Wallace, K., Burt, A.D. and Wright, M.C., 2008. Liver fibrosis. Biochemical Journal, 411(1), pp.1-18.
Zeybel, M. and İdilman, R., 2018. Serum biomarkers for the evaluation of liver fibrosis: The need for better tests. Turk J Gastroenterol, 29, pp.377-8.