Week 1: Complex wounds
Scenario 1:
Situation: Mr. Jennings, a 67-year-old male and he was presented with emergency laparotomy on day 4 post-operatively with a midline abdominal incision. He has a medical history of T2DM. Obesity, hypertension, and osteoarthritis.
Collect Cues
·T2DM, hypertension, and others indicate a complex medical history. His medication regimen includes Metformin, Paracetamol, and Lisinopril.
·Vital signs reveal: BP: 132/88 mmHg, RR: 22 bpm, Spo2: 95% on room temperature, HR: 104 bpm, and the body temperature was Temp: 38.3°C. Wound swab has been requested to order.
·Indicates post-operative complications or pulmonary embolism
Processing
·Data analysis confirms that the patient has fever and elevated heart rate, and RR reveals potential infection.
·Vital signs monitoring and wound assessment are highly relevant, but reviewing medical history in this case might not be relevant (Vyas et al., 2024).
·Indicates post-operative complication.
·Strong connection to wound infection or Pulmonary embolism.
Issues Actual issue would be PE or wound infection, whereas potential issues might be sepsis or organ failure.

Goals
·To treat the patient’s complications effectively.
·To achieve the treatment outcome by stabilizing the RR and HR within the next 2 hours by 40%.
·Collaboration with the healthcare professionals to implement tests to develop a treatment plan.
·Recognizing the urgency as a response to the patient’s clinical deterioration.
·Completing the entire treatment diagnosis within the next 2 hours.
Action:
·Informing the healthcare team.
·Diagnostic tests, including X-ray, CBC, and others.
·Giving antibiotics to manage pain.
Evaluate
·Monitoring signs and symptoms.
·Observation checklists to evaluate the effectiveness of the treatment.
Reflect:
·Opportunities related to the improvement of clinical deterioration through a strategic roadmap have been identified.
·Understanding the importance of collaboration with the medical team.


Scenario 2
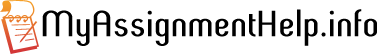
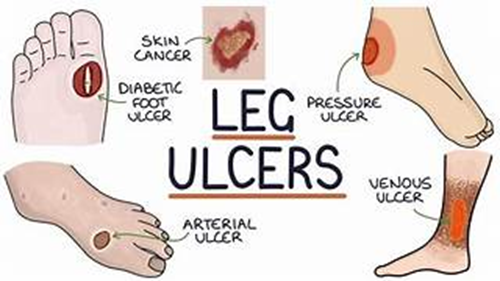
Situation: Mrs. Marino, a 74-year-old female, reported to the hospital with a venous leg ulcer on the portion of medial left portion of the ankle.
Collect Cues
·Venous leg ulcer that worsened over the past 2 weeks, history of hypertension, venous insufficiency, and DVT. The medication regimen includes Paracetamol, Amlodipine, and Aspirin.
·BP: 142/86 mmHg, RR: 18 BPM, HR: 88 bpm, SpO₂: 97% on room air. Her wound becomes red, with moderate serous exudate, and maceration of her peri-wound skin.
·The symptoms and vital assessment confirm that it might be the exacerbation of the symptoms of a leg ulcer, for which wound management will be necessary.
Processing
·Marino’s wound site does not heal as per the expectations.
·Wound assessment as well as medical history would be relevant in this case, as they are the common symptoms of venous insufficiency, while medications had no direct relevance to her current situation (Tan et al., 2024).
·Reveals chronic wound complications.
·Prompt intervention will be necessary by focusing on her wound site to prevent sepsis and other conditions.
Issues
·Her wound is worsening with maceration and increased exudate.
·Risks include decreased mobility, infection, or amputation.


Goals
·To improve her wound healing to prevent complications.
·To lower the wound exudate by 50% with wound dressing within 1 week and 80% within 2 weeks.
·Collaborating with the medical team.
·To recognize risk factors and triggers.
·To complete the wound management plan within the next 2 weeks.
Action:
·Wound management plan
·Collaboration with other professionals.
·Patient’s education
Evaluate:
·Monitoring healing by observing the wound.
·Depth measurement will be used to evaluate the healing effectiveness.
Reflect:
·Identification of the importance of wound management, especially when patients have a history of VI.
·Understanding the importance of the involvement of the health professionals.
Scenario 3
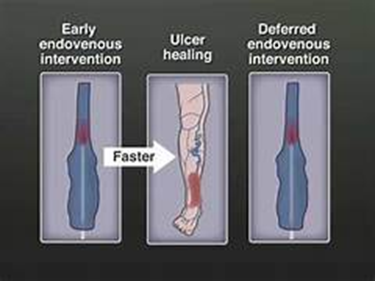
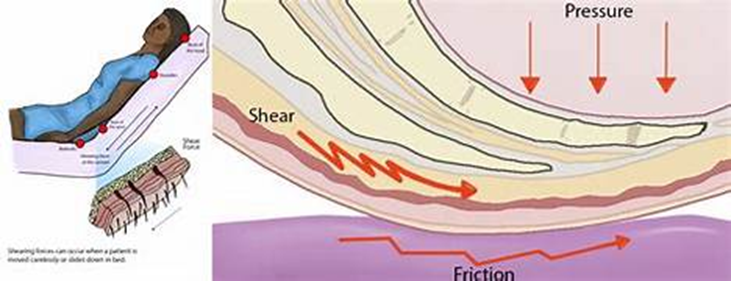
Situation: Mr. Cadwell, an 81-year-old male, presented to the hospital with stage 3 PI (Pressure injury) over the sacrum.
Collect Cues
·PI stage 3, situation worsening over 10 days, medical history of Parkinson’s disease, Y2DM, heart disease, and mild cognitive impairment. The medication regimen includes Bisoprolol, Metformin, and Clopidogrel.
·BP: 126/78 mmHg, SpO₂: 96% on room air, HR: 96 bpm, and RR: 20. Wound had moderate exudate slough, and skin was fragile.
·Pressure injury management is necessary for him, as he has limited mobility, which can further exacerbate the risks of PI.
Processing
·No healing of PI
·Medication review was less relevant than wound assessment and evaluating the medical history (Hess, 2019). Medical history provides conditions that might be risk factors for patients, while wound assessment will help to understand the characteristics of the wound to proceed with further treatments.
·Pressure injury can be complicated based on the patient’s vital signs monitoring and wound assessment, along with history.
·Immediate attention is required.
Issues
·PI is worsening, which is an issue, but it can further initiate sepsis or multi-organ failure as a potential complication.

Goals
·To improve the PI healing to lower the risks of sepsis.
·To measure would exudate and to boost healing by 60% within 1 week.
·Collaboration with the healthcare team.
·To address the severity of the PI management.
·To complete the entire purpose within the 2 weeks.
Action:
·Wound dressing and cleaning
·Educating the patient and his family members to promote health literacy.
Evaluate: The Bates-Jensen Wound Assessment Tool will be used to measure the progress or deterioration after implementing the action plan.
Reflect:
·Addressed the importance of pressure injury management.
·Understanding the complex situation that the patient might face if left untreated.

Week 2A: Care of the person with altered blood sugars (scenario 1)
Situation: Mr. Brown, a 50-year-old male, presented with T2DM and was admitted to the hospital 2 days ago due to a lower respiratory tract infection.
Collect Cues
·Medical history of hypertension, obesity, as well as T2DM.
·Medication regimen includes mixed insulin, Lisinopril, and metformin.
·BGL level: 19.4 mmol/L, no visible wound, but the patient experiences severe thirst and fatigue.
·Diabetes management is crucial, especially when BGL fluctuates.
Processing
·BGL is high, and he might be affected by hyperglycaemia.
·BGL, vital signs, and medication doses are all relevant aspects in this case.
·Immediate intervention.
·Treatment adherence to avoid harmful consequences.
Issues
·While BGL level shows hyperglycaemia, a risk for the patient; however, it can initiate diabetic ketoacidosis if left untreated (Berbudi et al., 2020).

Goals
·To manage hyperglycaemia
·To lower the BGL level from 19 to 4-10 mmol/L within the next 3 hours.
·Collaborating with the healthcare team.
·Recognizing the complexities.
·To complete the entire intervention plan within the next 3 hours.
Action:
·Administering medications and mixing insulin doses.
·Providing education on diabetes complexities.
Evaluate: Monitoring BGL level until it reaches the expected outcome.
Reflect:
·Understanding the importance of addressing risk factors that trigger the BGL level to become high. The importance of vital signs monitoring has been addressed.


Scenario 2
Situation: Mrs Julie Nguyen, who was a 72-year-old lady, was admitted with wrist pain, which was mild, along with hypoglycaemia.
Collect Cues
·History of T2DM and chronic kidney disease.
·BGL was 2.8 mmol/L.
·Experienced fatigue and light-headedness
Processing
·Low BGL indicates hypoglycaemia. Therefore, requiring clinical assistance.
·BGL, vital signs, and other reports are quite relevant in this case.
·Immediate intervention.
·Hypoglycaemia can be life-threatening, for which instant focus will be necessary to manage complications (Harding et al., 2024).
Issues: Hypoglycaemia is one of the issues that the patient faces, which further creates potential complications, including coma and even death.

Goals
·To manage hypoglycaemia to prevent risks.
·To achieve BGL level within the target range (4-10 mmol/L) within 30 minutes.
·Effective collaboration with professionals.
·Understanding the urgency of the intervention
·To complete the plan within the next 30 minutes.
Action:
·Glucose administration.
·Patient’s evaluation
Evaluate: Constant monitoring of vital signs to ensure safety.
Reflect:
·Knowledge and facts related to hypoglycaemia have been understood.
·The value of involving the medical team as a response to clinical deterioration has been addressed.
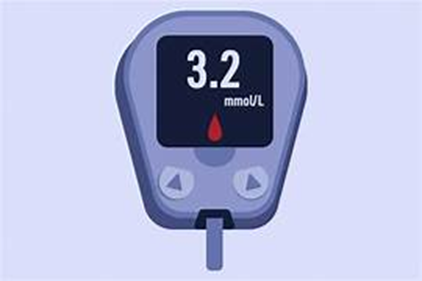
Scenario 3
Situation: A patient, named Mr. Wallace, a 76-year-old male admitted with increasing confusion and dehydration,
Collect Cues
·History of T2DM, heart failure, cognitive decline, and others. Metformin is used for T2DM with other medications (Furosemide and Amlodipine).
·BGL: 27.8 mmol/L, patient reported dry lips, poor skin, and weak pulses, urine output from vital assessment showed 300mL of concentrated, along with dark urine.
·Managing hyperglycaemia. BP was 98/58 mmHg, revealing hypotension.
·All of the assessments are relevant to ensure the root cause of his condition.
·Immediate attention.
·Hypoglycaemia can be risky and needs to be prioritized.
Processing:
·BGL level elevated.
·Requiring immediate action.
·BGL, vital signs, and urine output are highly relevant in this case.
Issues: Risk of having DKA or sepsis (Gosmanov et al., 2021).


Goals
·To manage hypoglycaemia as well as dehydration.
·To lower the BGL level from 27.8 to 4 or 10 mmol/L within the next 3 hours.
·Collaboration with experts.
·To recognize the severe complications that can be risky for the patient.
·To complete within the next 2 to 3 hours.
Action:
·IV administration
·Antibiotic therapy to suppress UTI.
Evaluate: Monitoring BGL level and patient’s hydration status.
Reflect:
·Understanding the risks after developing hyperglycaemia
·Understood the importance of focusing on communicating with healthcare experts during MET activation.

Week 2B: Endocrine (Scenario 1)
Situation: Mrs Helen, a 63-year-old woman, reported to the hospital due to her recent fall, and she was previously diagnosed with Graves’ Disease.
Collect Cues
·HR 130 bpm, RR 24 bpm, and BP 148/88 mmHg, and Spo2 level was normal (97%). She experienced symptoms including restlessness, weight loss. Palpitations, insomnia, and others. Medications include Propranolol to manage thyroid, Carbimazole, which also works to inhibit the synthesis of thyroid hormone, which affirms that, patient has hypothyroidism.
·Polyuria and thirst confirm mild dehydration or hyperglycaemia.
·Graves’ disease is a common outcome for patients with thyroid issues due to the stimulation of autoantibodies.
Processing
·HR: 130 bpm, sweating, and weight loss are symptoms that recommend worsening of hyperthyroidism. Excess thyroid hormone might enhance the tendency towards restlessness and insomnia as a neurological symptom.
·Most important cues are considered as tremors, anxiety, excessive thirst, and others, whereas Spo2 levels and temperature are less critical to the patient.
·Polyuria might be considered a side effect of hyperthyroidism without including diabetes.
·Her fall incidence might be related to tremors, tachycardia-induced dizziness, or fatigue.
·This report is consistent with the aspect of poorly controlled Graves’ disease instead of any pharmacological treatment.
·If left untreated, the patient can face the risk of cardiac failure.
Issues
·Hyperthyroidism
·cardiovascular instability Fatigue and fall risk

Goals
·To stabilize the heart rate by monitoring the cardiac output.
·To measure the heart rate to ensure it will reduce from 130 to below 100 within 10 minutes to avoid tachycardia.
·To collaborate with GP immediately to implement the plan
·Monitoring heartbeat for 30 minutes for the next 2 days.
·To stabilize the patient’s condition within 2 days.
Action:
·Notifying the entire medical team regarding the worsening situation.
·Performing ECG monitoring
·Monitoring fluid intake.
Evaluate: Monitoring patients’ vital signs by observing sleep cycle, tremors, fatigue, and other symptoms after 3 days.
Reflect:
·Early recognition of deterioration is necessary, which has been understood from this scenario.
·Vital signs abnormalities must be considered as endocrine crisis, even if the patient is stable.

Week 3: Hepatic (Scenario 1)
Situation: Mr. Collins, a 35-year-old male, presented with Hepatitis B infection, which was further confirmed by lab procedures.
Collect Cues
·His medical history confirms that he is quite fit but occasionally involved in alcohol usage. His medication regimen is paracetamol.
·BP: 110/68 mmHg, indicates normal, but the patient reported tallow eyes and the skin colour is like jaundiced skin, dark urine, and abdominal pain.
·Understanding the pathophysiology of the infection to develop treatment.
Processing
·Acute hepatitis B infection.
·The levels of bilirubin and liver enzymes are elevated.
·These are the common symptoms of Hepatitis B.
·Ongoing monitoring is necessary.
Issues: High levels of bilirubin and liver enzymes, which can be transmitted from his body to another (WHO, 2024).
Goals
·To manage his condition by preventing the illness from spreading.
·To reduce the level of liver enzymes within 3 weeks.
·To communicate with a healthcare professional.
·Understanding the importance of ongoing vital assessments.
·3 weeks will be the timeframe for the strategic treatment implementation.
Action:
·Antiviral therapy
·Patient’s education
Evaluate: Assessing the infection control measures to ensure to meet the objectives.
Reflect:
·Recognized the severity of hepatitis B infection, especially when patients are at high risk.
·Successfully understood to prioritize collaboration to release the overburden from the nursing staff.

Scenario 2
Situation: Mr Reyes, a 59-year-old male, reported with chronic hepatitis C along with liver cirrhosis.
Collect Cues
·Medical history; Chronic hepatitis B, T2DM, and liver cirrhosis. Medications include lactulose, metformin, and others.
·Patient’s report confusion as well as slurred speech.
·Cirrhosis
Processing
·Elevated ammonia is evidence that worsens liver conditions among patients.
·BP: 94/60 mmHg
·Lab results as well as clinical findings are relevant.
·Coagulopathy reveals hepatic encephalopathy.
·Immediate attention.
Issues
·Hepatic encephalopathy can initiate neurological risks as a potential complication (Oana Săndulescu et al., 2024).
·The risk of bleeding can be higher. Life-threatening complication.

Goals
·To manage hepatic encephalopathy
·To reduce the ammonia level within the next 20 hours by using lactulose.
·Collaborating with a medical professional.
·To address ongoing monitoring.
·20 hours.
Action:
·Lactulose administration.
·Monitoring the mental status of the patient.
·Provide supportive care
Evaluate: Monitoring mental status and vital signs
Reflect:
·Understanding hepatic encephalopathy as a risk factor that can be life-threatening if left untreated.
·Evaluated the importance of patients’ education.
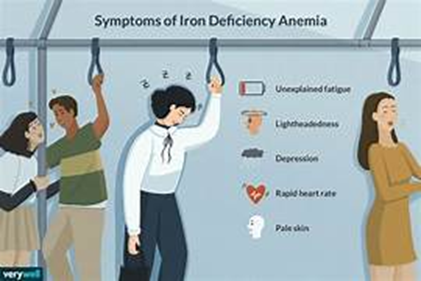
Scenario 3
Situation: Mr. Miller, a 74-year-old female, possesses a history of iron deficiency, osteoarthritis, and heart failure.
Collect Cues
·Her medication regimen includes ferrous sulphate, paracetamol, and furosemide.
·Experienced lower back pain, chest tightness, and feeling flushed.
·Must have knowledge of blood management for transfusion.
Processing
·Possible blood transfusion reaction noted from the vital signs.
·Clinical findings and vital signs are completely relevant in this case.
·Immediate attention will be necessary.
Issues
·Elevated body temperature, heart rate (112 bpm), and blood pressure (94/60 mmHg).
·Potential issues can be renal failure and cardiovascular issues.

Goals
·To manage haemolytic transfusion to safeguard the RBCs to prevent complications (Harewood and Master, 2023).
·To lower the body temperature while increasing BP, as it reveals hypotension within the next 30 minutes.
·Collaboration with healthcare staff to hinder blood transfusion.
·To recognize the requirement of blood transfusion management.
·30 minutes.
Action:
·Stopping blood transfusion
·Antipyretics administration
·Oxygen therapy and cardiac monitoring.
Evaluate: Monitoring vital assessment (A-E framework)
Reflect:
·Identification of the risk factors and triggers.
·Understood the contribution of the medical team in achieving positive outcomes for patients who are receiving blood transfusions.

Week 4: Renal (Scenario 1)
Situation: Mr Patel, a 46-year-old male, presented with the sudden onset of flank pain that further radiates to the groin.
Collect Cues
·No chronic medical history, but occasionally involved in NSAID use.
·No regular medications have been found.
·Patients reported nausea, dark urine, and elevated BP (138/88 mmHg).
·Having the presence of kidney stones and kidney injury.
Processing
· Analysis of the symptoms of renal colic along with the pain intensity of the patient.
·The medical analysis, reports, and urinalysis are the relevant focus.
·Severe flank pain, dark urine, and nausea are the common symptoms of kidney injuries or kidney stones (Patti and Leslie, 2021).
·Immediate attention is necessary
Issues
·Based on the patient’s situation, he might be affected by a kidney stone, which is an actual issue.
·From this, kidney injuries or renal failure can be expected as a potential threat.

Goals
·To manage his acute renal colic to avoid harmful consequences like dark urine and nausea.
·To reduce the pain intensity by using the pain score tool from 8/10 to 3/10 within 6 hours.
·To administer painkillers, IV fluids, and check vital assessments.
·To address the importance of early recognition of the health issue.
·To proceed with the plan and expect the outcome within the next 6 hours.
Action:
·Providing oral paracetamol
·IV morphine and fluid administration to relieve the pain.
·Monitor urinary output and other vital signs.
Evaluate: Pain score will be used as a tool to recognize the patient’s pain level to ensure the effectiveness of the treatment action.
Reflect:
·Patient education is important, which has been recognized by dealing with this patient.
·Identification of possible interventions to achieve a positive outcome.

Week 5:Altered Immune (Scenario-1)
Scenario 1
Situation: Mrs. Patricia, a 62-year-old woman, has been diagnosed with Stage III non-small cell lung cancer. She is about her first round of chemo and was admitted due to dehydration.
Collect Cues
·Medical history: mild COPD, anxiety, and NSCLC Stage III, as well as 40 years of smoking history.
·The medication regimen includes Salbutamol, Ondansetron, and others.
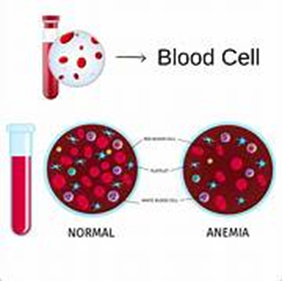
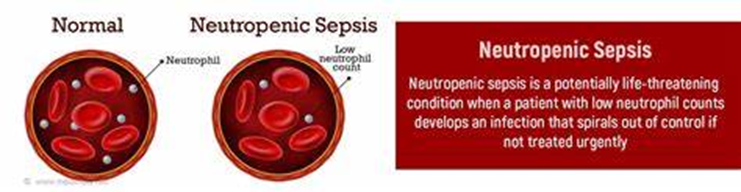
·She reported nausea, anxiety, and CBC confirms Neutropenia along with elevated creatinine.
·Chemotherapy triggers suppression of the bone marrow, which leads to fatigue
Processing
·Neutropenia elevates the risk of infection.
·Dehydration might be caused by poor intake or dry mucous membranes.
·No sign of allergies, which is irrelevant in this context, but low Hb, poor intake, and chemotherapy can be relevant.
·Chemotherapy induced adverse effects, including emotional distress, fatigue, and nausea.
·The scenario aligns with an aspect of the post-chemo symptom complex.
·Immediate attention will be necessary to lower the risk of acute renal injury.
Issues
·Poor oral intake
·Fatigue
·Risk for potential issues, including Neutropenia


Goals
·To prevent any sort of neutropenic sepsis
·To measure the electrolyte balance to reduce the symptoms by 80% within 2-3 days.
·To receive support from the healthcare staff to provide a positive outcome.
·To respond early to clinical deterioration.
·2-3 days
Action:
·IV fluid administration
·Maintaining hand hygiene for managing neutropenia as a precaution.
·Monitoring vital signs.
Evaluate:
·Monitoring the improvement signs
·Decreased nausea and fatigue while improving oral intake
·Stabilizing creatine level.
Reflect:
·Proactively screening to understand the emotional well-being of the patient.
·Understanding the importance of earlier collaboration with the GP and psychologist to manage the patient’s situation.

References
Berbudi, A., Rahmadika, N., Cahyadi, A. I., & Ruslami, R. (2020). Type 2 Diabetes and Its Impact on the Immune System. Current Diabetes Reviews, 16(5), 442–449. https://doi.org/10.2174/1573399815666191024085838
Gosmanov, A., Gosmanova, E., & Kitabchi, A. (2021). Hyperglycemic crises: Diabetic ketoacidosis (DKA), and hyperglycemic hyperosmolar state (HHS). National Library of Medicine; Endotext. [Accessed on: 15/7/25] Retrieved From: https://www.ncbi.nlm.nih.gov/books/NBK279052/
Harding, J. E., Alsweiler, J. M., Edwards, T. E., & McKinlay, C. J. (2024). Neonatal hypoglycaemia. BMJ Medicine, 3(1). https://doi.org/10.1136/bmjmed-2023-000544
Harewood, J., & Master, S. R. (2023, September 12). Hemolytic Transfusion Reaction. Nih.gov; StatPearls Publishing.[Accessed on: 15/7/25] Retrieved From: https://www.ncbi.nlm.nih.gov/books/NBK448158/
Hess, C. T. (2019). Comprehensive Patient and Wound Assessments. Advances in Skin & Wound Care, 32(6), 287–288. https://doi.org/10.1097/01.asw.0000558514.64758.7f
Oana Săndulescu, İmran Hasanoğlu, & Mojca Matičič. (2024). Updates in viral hepatitis in 2024 – summary of education, research and leadership activities of the ESCMID Study Group for Viral Hepatitis (ESGVH). GERMS, 320–321. https://doi.org/10.18683/germs.2024.1442
Patti, L., & Leslie, S. W. (2021). Acute Renal Colic. PubMed; StatPearls Publishing. [Accessed on: 15/7/25] Retrieved From: https://www.ncbi.nlm.nih.gov/books/NBK431091/
Tan, M., Lurie, F., Hernan Bauza Moreno, Van, D., Parsi, K., & Davies, A. H. (2024). Management of venous leg ulcers. Phlebology. https://doi.org/10.1177/02683555241243167
Vyas, V., Sankari, A., & Goyal, A. (2024). Acute Pulmonary Embolism. National Library of Medicine; StatPearls Publishing. [Accessed on: 15/7/25] Retrieved From: https://www.ncbi.nlm.nih.gov/books/NBK560551/
WHO. (2024, March 29). Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection. Www.who.int. https://www.who.int/publications/i/item/9789240090903